One of the challenges with measure validation is determining if all workflows have been mapped. Selecting patients only in the denominator can uncover issues, however many patients may need to be validated before finding missing workflows or identifying other issues. The larger the center, the more patients this may take.
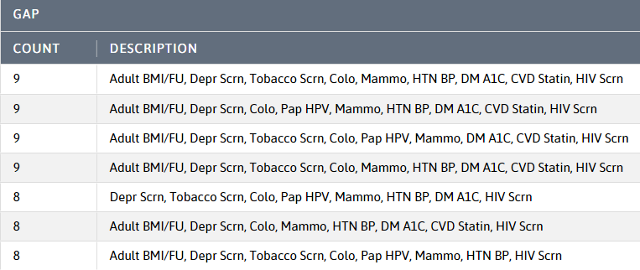
The DRVS UDS 2021 CQMs - Care Gaps report, shown below, is an excellent tool for measure validation. Though the temptation may be to validate patients with the most gaps, since multiple measures can be validated by looking at one chart, there is a more efficient approach.
Model Patients
Model patients are patients that have only one care gap because they are on top of their health care. This is especially true for patients that have cancer screenings but are missing something that can be completed in the office (e.g. BMI and follow-up).
To see model patients:
- Run the Care Gaps Report (ReportsUDS 2021 CQMs – Care Gaps).
- Filter the count to patients with 1 gap.
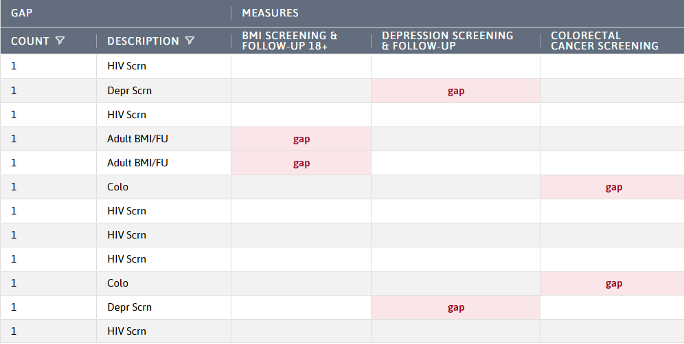
- Focus on a specific measure by filtering the description to the measure being validated or filter to the gap in the measure heading.
- Validate patients to identify a missing workflow, discover a workflow issue and/or gain confidence in the measure. Typically, 10-15 patients are needed.
This method can also be used to perform a deeper dive into a specific provider or location. The first step is to identify a provider or location that has lower than expected measure results. This can be done by following these steps:
- Run the measure analyzer for the measure of interest.
- In the comparison chart, group by Provider - Rendering or Location - Rendering.
- Change to the table view and sort the denominator in descending order.
- Look for low results amongst similar denominators.
In the example below, the providers with the largest denominator have the best results. The results go down on provider number 5 and then plummet. This could indicate that the last two providers or their MAs need training or that they are using a workflow that is not mapped. Go back to the care gaps report, filter to one of the providers, measure and care gap = 1. Validate a sample of the displayed model patients.
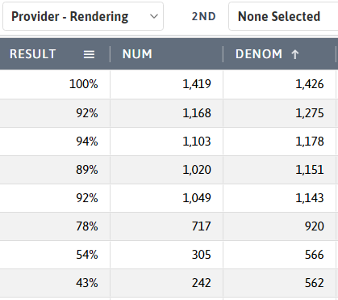
If a workflow is not being followed, it can be treated as a training opportunity.
If the data is recorded in a structured way in the EHR but is not available in DRVS, submit a ticket to Azara Support. Be sure to include a sample MRN and a screen print of the recorded item for that MRN.
Another use of this approach is to reach out to patients with one gap and no upcoming appointment. These patients may be more receptive to coming into the CHC to close the gap. This targeted approach can help bring up a specific measure result.
To validate the depression remission measure, use the year period in measure analyzer or the measure validation workbook.
The measure analyzer or measure validation workbook should also be used for the child measures. There are only 2 UDS measures for children on the care gaps report and there are different age ranges for each.
It is never too early to start looking at the UDS measures.
If you would like to work closely with an Azara staff member on your UDS validation, please contact your PCA, HCCN or Azara Account Rep at solutions@azrahealthcare.com.
Related Articles

The Road to UDS+: Past, Present, and Future
Explore Insights
UDS “Season” 2023/2024 is in the books!
Explore Insights
