September is Suicide Prevention Awareness Month. With suicide rates increasing 36% from 2020-2021 and being the 12th overall leading cause of death in the United States, it is never too soon to think about what role care teams can play in reducing that rate. In this blog, I want to take the opportunity to talk about one tool in the Azara DRVS tool belt to help identify patients who are most at risk.
Identifying Risk Factors
Studies show that only 46% of people who die by suicide had been previously diagnosed with a mental health condition. I was shocked by this statistic, and it got me thinking about how to identify potential warning signs for the other 54%. These studies have also provided insight into other risk factors that may indicate a patient is at increased risk of suicide.
In population health, we know disparities to be an important factor in healthcare, and like many other health conditions, suicide risk is no exception. Race, sexual orientation, social drivers of health, to name a few, are all factors that increase the risk of suicide. The highest rates of suicide in the U.S. are among American Indian/Alaskan Natives and non-Hispanic whites. Lesbian, gay, and bisexual youth are 4 times more likely to attempt suicide than straight youth, and transgender adults are 9 times more likely to attempt suicide than the general population.
How DRVS Can Help
Studies have concluded that a diagnosed mental health condition is not the only indication that a person is at increased risk for suicide—they have also uncovered trends for other risk factors. Having this knowledge and access to patient data empowers us to provide services to a broader at-risk population. Utilizing the tools Azara DRVS has to offer can help flag patients who do not have a mental health diagnosis but could still be at high risk. With the services care teams provide and the functionalities available in DRVS, we can come together as a community to play an important role in prevention.
If you’ve been a DRVS user for any length of time, I am sure you know that there are countless ways to manipulate the data that is already available, whether it be creating a custom registry or dashboard, or applying filters to reports and measures—all of which allow you to run reports focused on specific patient populations.
While the above are all great ways to manipulate the data available in DRVS, the tool I want to talk about today is Cohorts and more specifically Dynamic Cohorts. Dynamic Cohorts can be instrumental in tracking patients based on set characteristics that may increase their risk of suicide.
Cohort Basics
Let’s start with the basics—what is a Cohort? A Cohort is a group of patients that meet a set criteria, and in DRVS can be used to apply to Reports, Measures, or Registries as a filter, appear on the banner of the Patient Visit Planning (PVP) Report or be used in Azara Care Connect.
There are three types of Cohorts available in DRVS:
Static Cohort – Static Cohorts are part of core DRVS and do not require additional implementation. These require manual entry and removal of patients. They need to be maintained and updated manually to reflect the most accurate data. While effective, they can be cumbersome to maintain an accurate reflection of patients who meet the set criteria.
DRVS Dynamic Cohort – These are stock Cohorts that have been created using observations and data points that already exist in DRVS, such as blood pressure readings, labs, etc. to create inclusion and exit criteria. They do not require additional implementation.
Example:
DRVS DYN Depression/Anxiety Cohort: DRVS will dynamically enter any patient who has a diagnosis of depression or anxiety into this Cohort. If a patient no longer meets these criteria or is deceased, they are automatically removed from the Cohort.
EHR Dynamic Cohort – This Cohort is custom, created with our help using structured data that is in your EHR to create both the entry and exit criteria for the Cohort. This provides the ability to customize the patient populations that are most important to track and monitor. Keeping with the theme of unveiling patients who may be at risk and under the radar, Cohort criteria could include demographic data, in addition to an elevated PHQ9, or history of domestic violence or housing insecurity. Another option would be to have the Cohort created to include only patients who fall into the 46% with a mental health diagnosis, or better yet, a Cohort that looks at both these sets of entry criteria to allow for tracking patients who fall into either criteria.
Example:
Suicide High Risk Cohort:
- Entry Criteria 1: PHQ-9 > 10 AND LGBGT+ OR substance use
Or
- Entry Criteria 2: History of mental illness, OR previous suicide attempt
- Exit Criteria: Behavioral health visit AND a high-risk suicide screening response of No after the date above entry criteria was met
We would work with you to capture this data from your EHR to be used in this Dynamic Cohort so patients would enter and exit dynamically based on these criteria with no need for manual entry.
Cohorts in Action
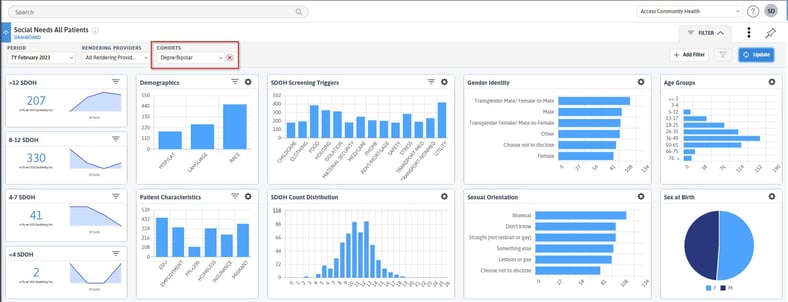
Pictured above is an example of a Social Needs Assessed Dashboard with a Cohort filter applied for a visualization of patients included in the Depression/Bipolar Cohort. This exemplifies how this filter can be applied to track specific populations across various measures in DRVS.
%20-%20Cohorts.jpg?width=822&height=223&name=Patient%20Visit%20Planning%20(PVP)%20-%20Cohorts.jpg)
Above is an example of Cohorts displayed on the PVP Banner. The prefix Dyn before the Cohort name indicates the Cohort is dynamic.
Dynamic Cohorts in DRVS can be an easy way to alert you of risk factors for patients at the point of care and beyond. And while I chose to highlight how they can be used toward suicide prevention efforts, I hope this information got you thinking about the various use cases for Cohorts in your practice.
How to Enable Dynamic Cohorts
If you have any questions about Cohorts or are interested in learning more about Dynamic Cohort options, please open a ticket with Azara Support.
Want to learn more about how Azara can help your organization meet it’s population health and value-based care goals? Contact solutions@azarahealthcare.com or request a demo now.
Sources:
National Alliance on Mental Illness, Suicide Prevention Awareness Month (SPAM)
https://www.nami.org/Get-Involved/Awareness-Events/Suicide-Prevention-Awareness-Month-(SPAM)
Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, November 2022
https://www.cdc.gov/suicide/factors/index.html
Related Articles

Value-Based Care Foundations Part 2: A New Chapter in Risk Adjustment
Explore Insights
Socioeconomic Status, Access, and Control: Rethinking Diabetes Outcomes
Explore Insights
