Back in 2016, Azara published two blog posts on the difference between the two ways diagnoses are added to a patient’s chart (problems and assessments) when to use them, and the impact this has on clinical quality measures. As DRVS has evolved to use diagnosis data in new ways, this topic is worth an update, and we’ll do so by covering the difference between Problems and Assessments, look at the impact of this difference on clinical quality measures through a patient example, and then review how DRVS displays diagnoses.
Problems Versus Assessments
An assessment documents a diagnosis which is present or addressed at the time of the visit: a codified version of the “reason for visit” entered during scheduling. 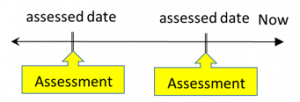 This could include chronic conditions like diabetes (E11.*), acute conditions like a broken arm (S52.*), Symptoms like wheezing (R06.2), procedures such as a pregnancy test (Z32.*), or even dietary counseling (Z71.3). In general, assessments are used as the justifying diagnosis for any charges associated with a visit, and so they get sent to health plans, lab vendors, and HIEs alike. Assessments are also relatively simple data points, as there are only an assessed date and a diagnosis code. This means that assessments are associated with a visit, and pertain only to what occurred during that visit.
This could include chronic conditions like diabetes (E11.*), acute conditions like a broken arm (S52.*), Symptoms like wheezing (R06.2), procedures such as a pregnancy test (Z32.*), or even dietary counseling (Z71.3). In general, assessments are used as the justifying diagnosis for any charges associated with a visit, and so they get sent to health plans, lab vendors, and HIEs alike. Assessments are also relatively simple data points, as there are only an assessed date and a diagnosis code. This means that assessments are associated with a visit, and pertain only to what occurred during that visit.
On the other hand, a problem documents a diagnosis that affects the patient for an extended period; a codified version of the specialty of care they are receiving. 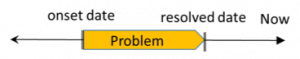 Problem lists used within health records are a list of illnesses, injuries, and other factors that affect the health of an individual patient, usually identifying the time of occurrence or identification and resolution. For example, both depression (F33.*) and history of mental disorders (Z86.59) would belong on the problem list.
Problem lists used within health records are a list of illnesses, injuries, and other factors that affect the health of an individual patient, usually identifying the time of occurrence or identification and resolution. For example, both depression (F33.*) and history of mental disorders (Z86.59) would belong on the problem list.
The advantages of adding a diagnosis as a problem are that it will follow the patient through the EHR on the problem list and it can have its onset, diagnosis, and resolved dates tracked as discreet data points. Since the problem can cover the time between visits, a problem is associated with the episode of care and doesn’t tell you whether a patient was treated for the condition at a specific visit.
Any certified EHR will support both of these methods, and health centers are strongly encouraged to document diagnoses in both ways when appropriate to avoid a wide range of issues. Inconsistent use of assessments can lead to rejected claims and reduced reimbursements, and inconsistent use of the problem list can lead to poor coordination of care across a team and difficulty determining which patients have certain chronic conditions. The example below gives a scenario for which this might happen.
Patient Example
Bonnie Bunny was diagnosed with hypertension three years ago by Dr. Farmer at Rabbit Community Health Center (RCHC). Dr. Farmer put her on ACE inhibitors two years ago to help manage her condition. Fifteen months ago she had her LDL tested because Dr. Farmer suspected high cholesterol was affecting her hypertension and last month’s visit was the 3rdone this year where her blood pressure was found to be in control.
Unfortunately, Dr. Farmer doesn’t do a good job of maintaining the problem-list, so Bonnie only has assessments for hypertension. As part of an Accountable Care Organization (ACO), RCHC receives clinical quality dollars for controlling the blood pressure of their hypertensive patient, but when RCHC’s Quality Improvement (QI) team looks at their “Hypertension Blood Pressure Control” measure, Bonnie is not included. Since she has her blood pressure in control, the QI team wants to ensure that patients like her are included in the measure as they will have a positive impact on the measure result.
So why is she not being counted as having hypertension?
To understand why Bonnie is not being counted in the hypertension measures, we need to focus on what the difference is between an assessment and a problem. An assessment documents a diagnosis which is present or addressed at the time of the visit while a problem documents a diagnosis that affects the patient for an extended period. With this difference in mind, let’s go back to the example of Bonnie Bunny. From a measure logic perspective, her hypertension diagnosis at RCHC looks like this:
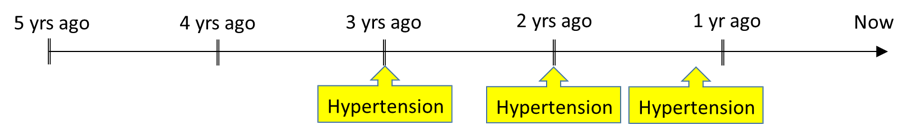
With only assessments in Bonnie’s chart, her hypertension diagnosis takes the form of a series of points where she received care for hypertension. But since her last assessment was 15 months ![]() ago for an LDL test, if you searched for patients with “active hypertension” in the past year, she would not be included.
ago for an LDL test, if you searched for patients with “active hypertension” in the past year, she would not be included.
A patient with hypertension whose BP is in control would be in the numerator of the “Hypertension Blood Pressure Control” measure. But since a problem of hypertension is not documented, the patient is not being counted in the denominator and presents as a negative impact on the center’s measure performance. Imagine if Dr. Farmer had recorded Bonnie’s diagnosis as a problem alongside the assessment when she was first diagnosed three years ago. As an active problem, the diagnosis is open-ended, and from a measure logic perspective, her hypertension diagnosis at RCHC would now look like this:
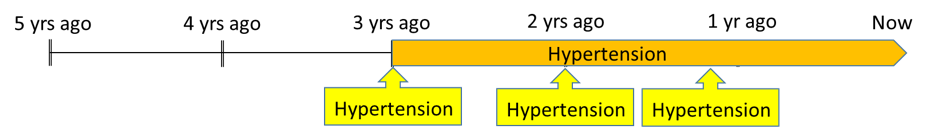
With this change, if you look for patients with “active hypertension” in the past year, she would show up in the denominator because of the active problem. This way RCHC still gets credit for the care they’ve provided to Bonnie in the past, and the benefits of a treatment that has occurred over the past three years.
By adding the problem, the provider is documenting the fact that the patient has well-controlled hypertension, even if they have not had that problem addressed at a recent visit. Proper use of problems allows the patient’s chronic conditions to be better managed by the care team and ensures appropriate patients are included in a measure. This is especially true for patients with chronic conditions, when improvements in the patient’s health, e.g., controlled blood pressure, is the result of a course of treatment that has been established and monitored over time.
How DRVS Displays Diagnoses
One of the core tenets of DRVS is that when you are shown the result for a clinical quality measure, relevant patient detail for that measure is provided to ensure a health center’s population is being correctly reflected. For any measure that includes diagnoses as part of the denominator, numerator or exclusion criteria, a diagnosis date, and the code will be relevant and therefore included in the measure patient detail.
Given all we’ve discussed above, how does DRVS chose a diagnosis code and date to display given that a patient might have multiple overlapping problems and assessments for the same measure?
At the basic level, our goal is to display the diagnosis data which qualified the patient for the measure for the longest period of time. In practice, this means that DRVS will display the ICD9/ICD10/SNOMED code and onset date for the earliest diagnosis which was active during the period. Many measures look for problems that were active in the period even if it was resolved before the end of the period. Therefore, an inactive problem will still qualify a patient, for a measure.
This is a good reason to accurately record when a condition on the problem list was resolved. When the resolved date of a problem is relevant to the measure itself, then we will display that in the patient detail. Otherwise, the diagnosis will only have a diagnosis date, which is the onset date.
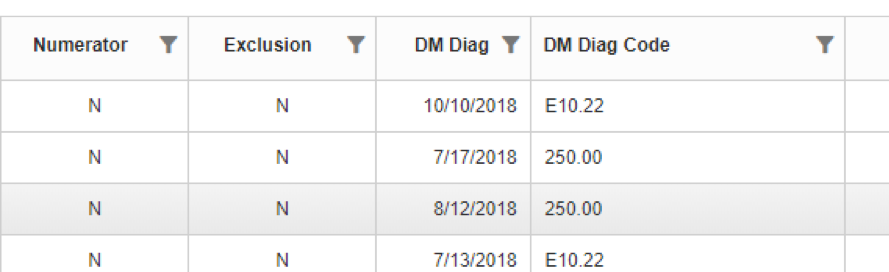
In the above example of Bonnie Bunny, we could expect that the code and onset date of the problem would appear in the patient detail since it was the only active diagnosis record in the period. But even if Bonnie had an assessment for hypertension within the year, the problem would still be displayed since it had been active for the longest period of time.
This process helps clarify why a patient is in a measure and identifies whether a patient is newly diagnosed or has been in care for some time which can be helpful for managing their treatment plan.
Hopefully, this discussion helps you to understand the role of problems and assessments in the measurement world of DRVS. If you have further questions, please reach out to us at support@azarahealthcare.com
Want to learn how Azara can help your organization meet it’s population health and value-based care goals? Contact solutions@azarahealthcare.com or request a demo now.
Related Articles

Value-Based Care Foundations Part 2: A New Chapter in Risk Adjustment
Explore Insights
Socioeconomic Status, Access, and Control: Rethinking Diabetes Outcomes
Explore Insights
