Value-Based Care Reporting with Payer Integration
Azara empowers organizations to achieve better outcomes for their patients through a proven, scalable technology platform.

Azara delivers timely, actionable clinical insights to care teams that facilitate collaboration with health plans and other value-based care enablers.
This enables healthcare organizations to work hand-in-hand with health plans on critical initiatives like engaging attributed members in preventive care, improving clinical quality, capturing risk adjustment factors, and driving performance improvement. By equipping providers with up-to-date actionable information and streamlining risk gap closure and the sharing of supplemental data, Azara fosters a collaborative environment where all stakeholders can work together to monitor, track, and improve quality, cost, and utilization outcomes for the entire patient population.
Azara seamlessly integrates health-plan provided data, such as rosters and claims from multiple plans, within existing workflows. This unified dataset enables member-focused programs to optimize quality measures, close risk and care gaps, and precisely identify and target high-risk patients through risk stratification – all within the unified Azara DRVS platform.
Azara DRVS further supports value-based care success with an experienced Clinical Transformation team and a comprehensive library of over 600 measures – including over 50 certified HEDIS® measures, CMS eCQM measures used for MSSP, MCP, & PCF programs, and a broad range of other clinical quality measures, covering all health plan members.


Organizations use Azara solutions to engage with health plans and members – improving care by enabling providers to:
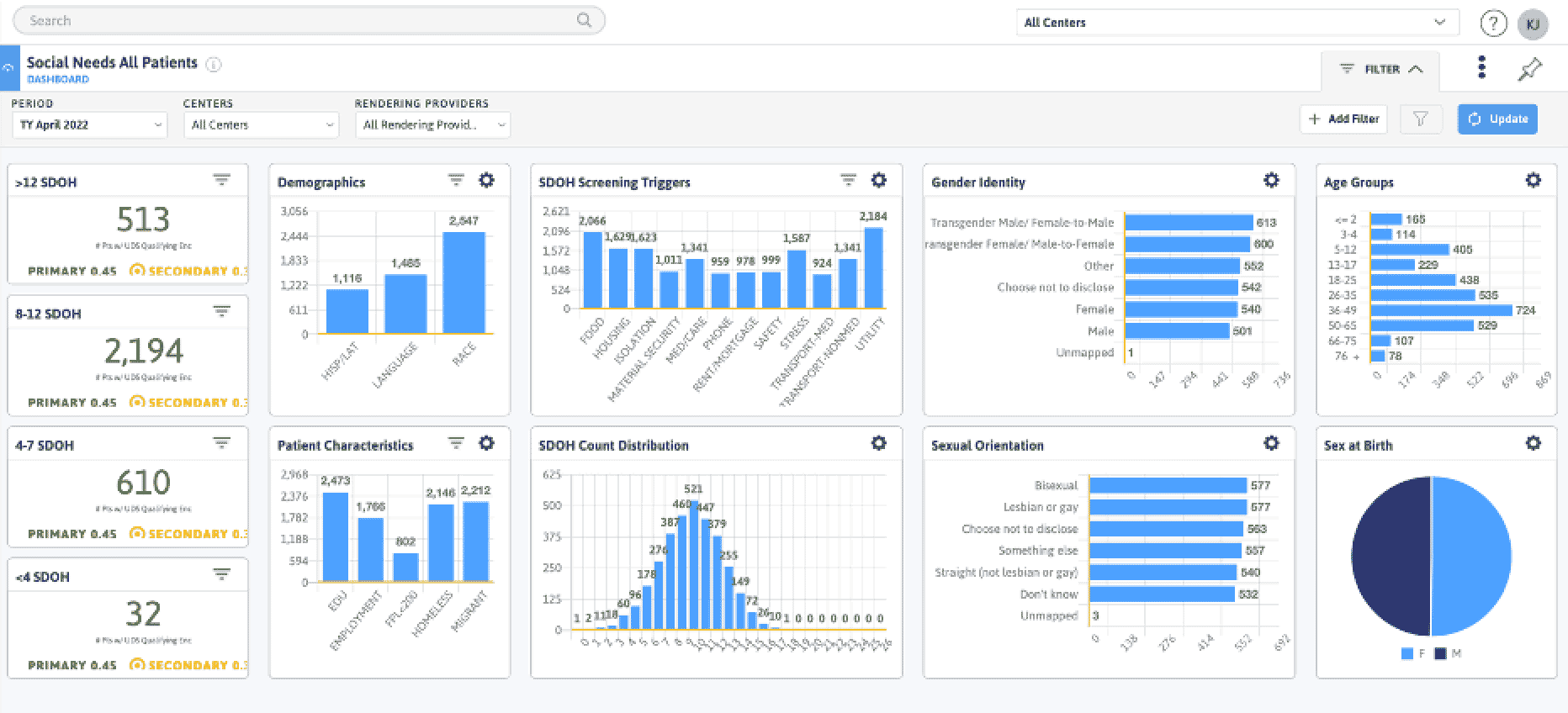
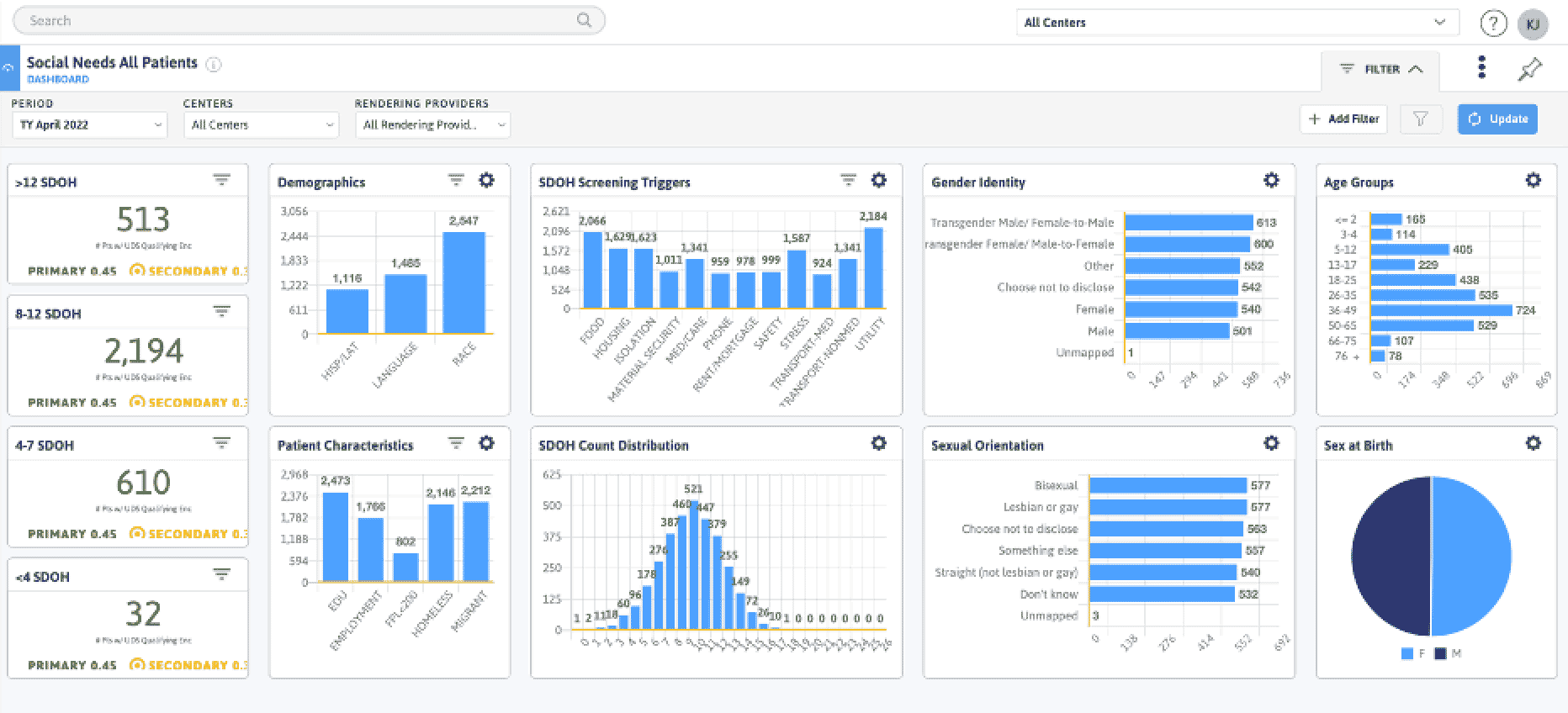
Unify member insights by aggregating and standardizing supplemental data directly from health plans – empowering care teams with a comprehensive and timely understanding of patients' conditions and risk factors.
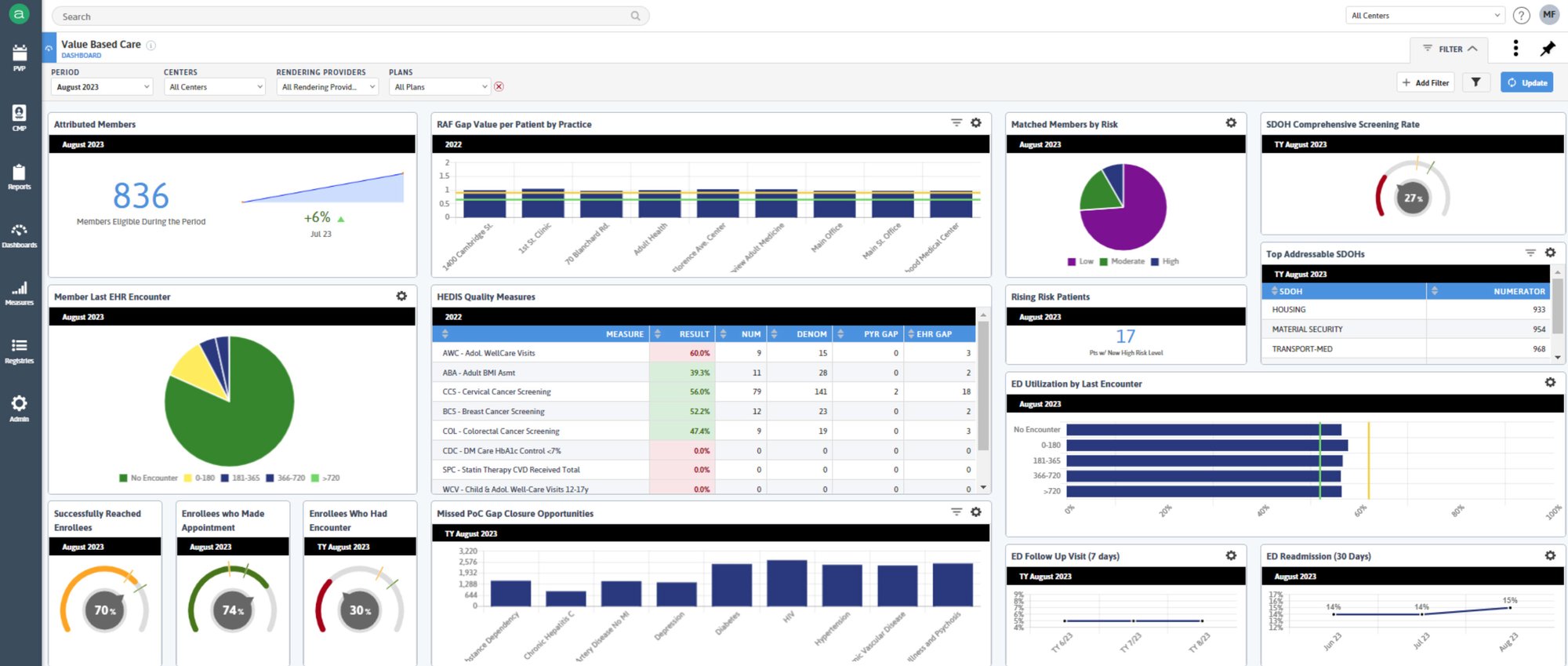
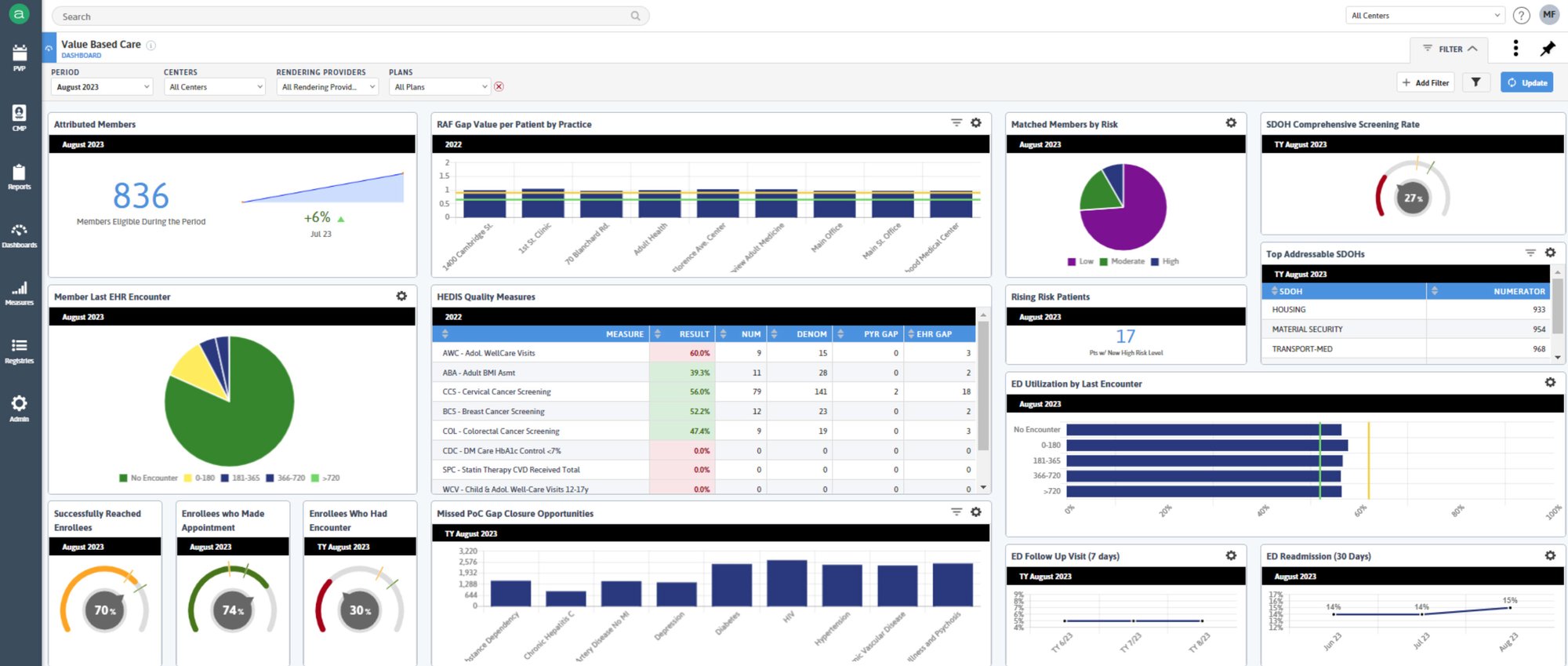
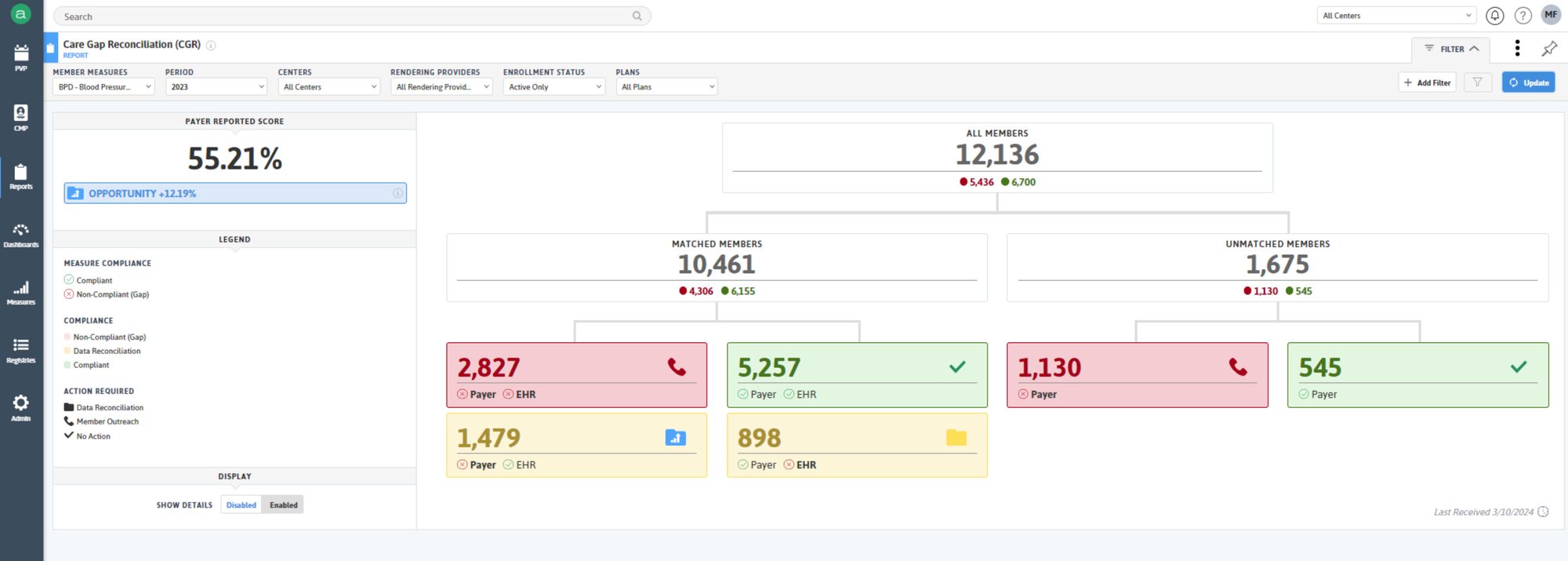
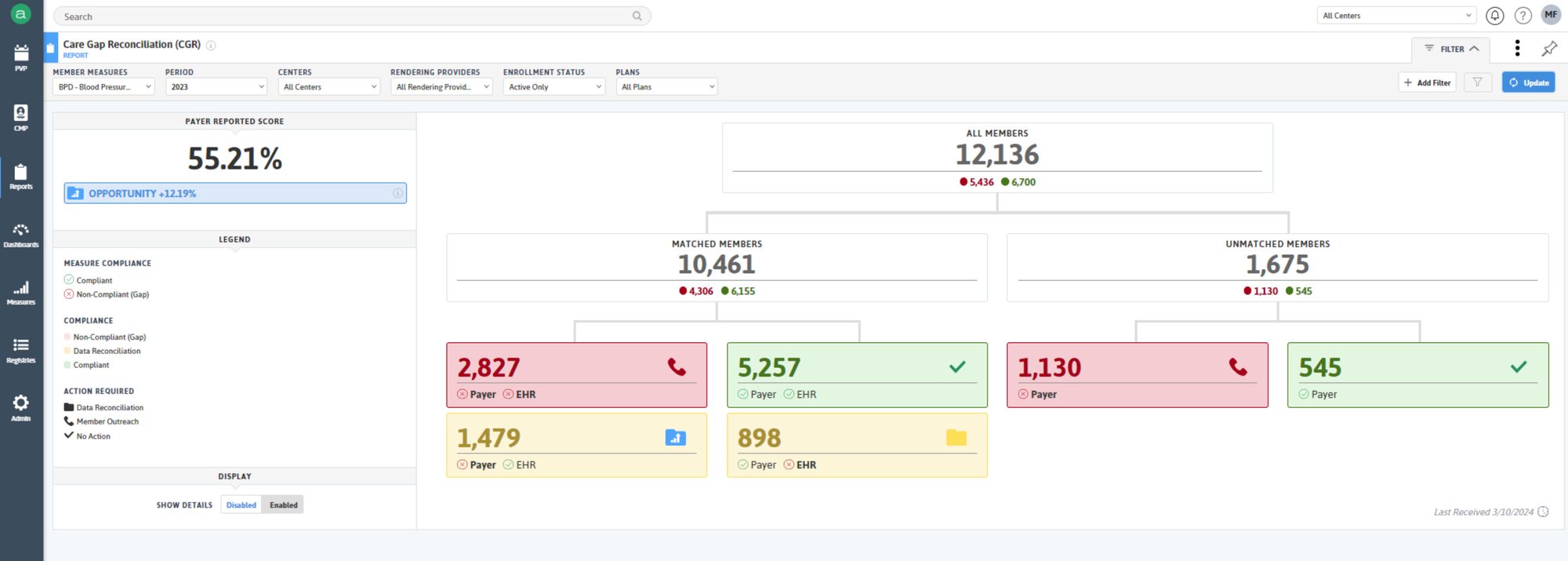
Significantly reduce wasted time and effort by closing care gaps with Azara's automated care gap reconciliation functionality which seamlessly matches payer-calculated gaps against EHR data – revealing the true status of gaps and ensuring resources are focused on the issues that matter most.
Access real-time risk stratification to continuously identify and address potential member health issues.
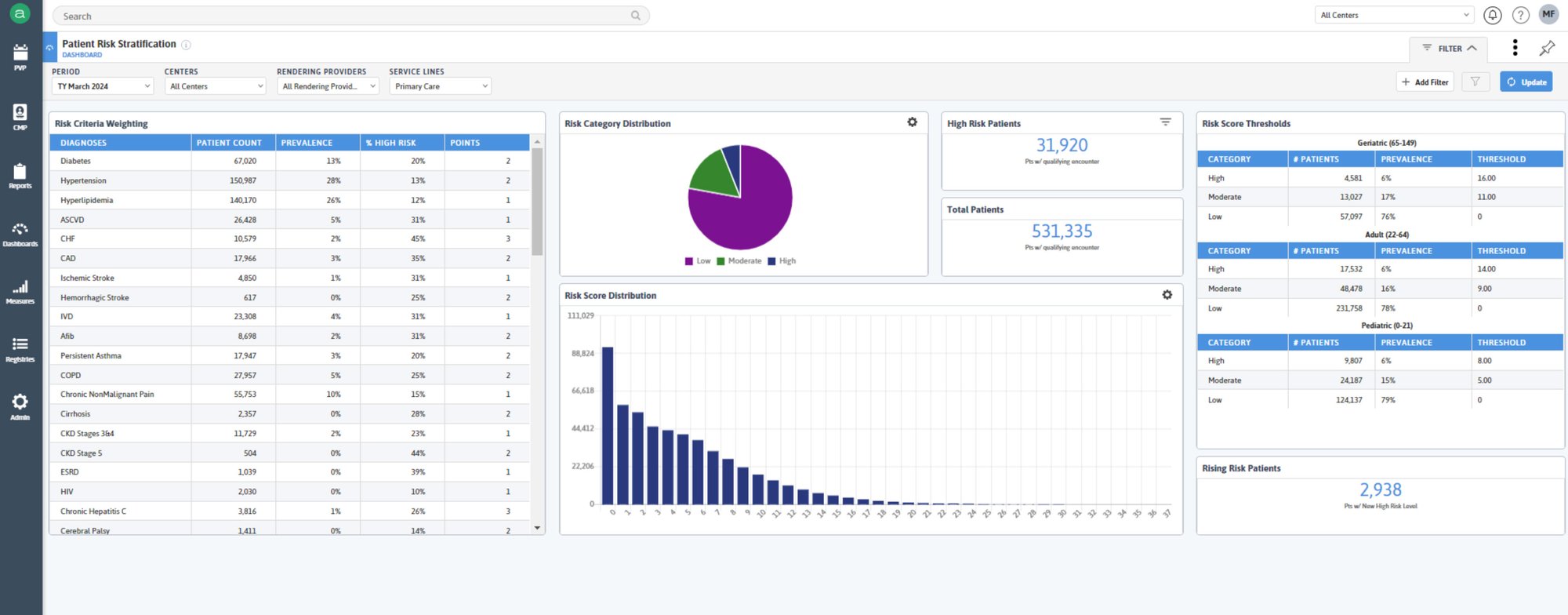
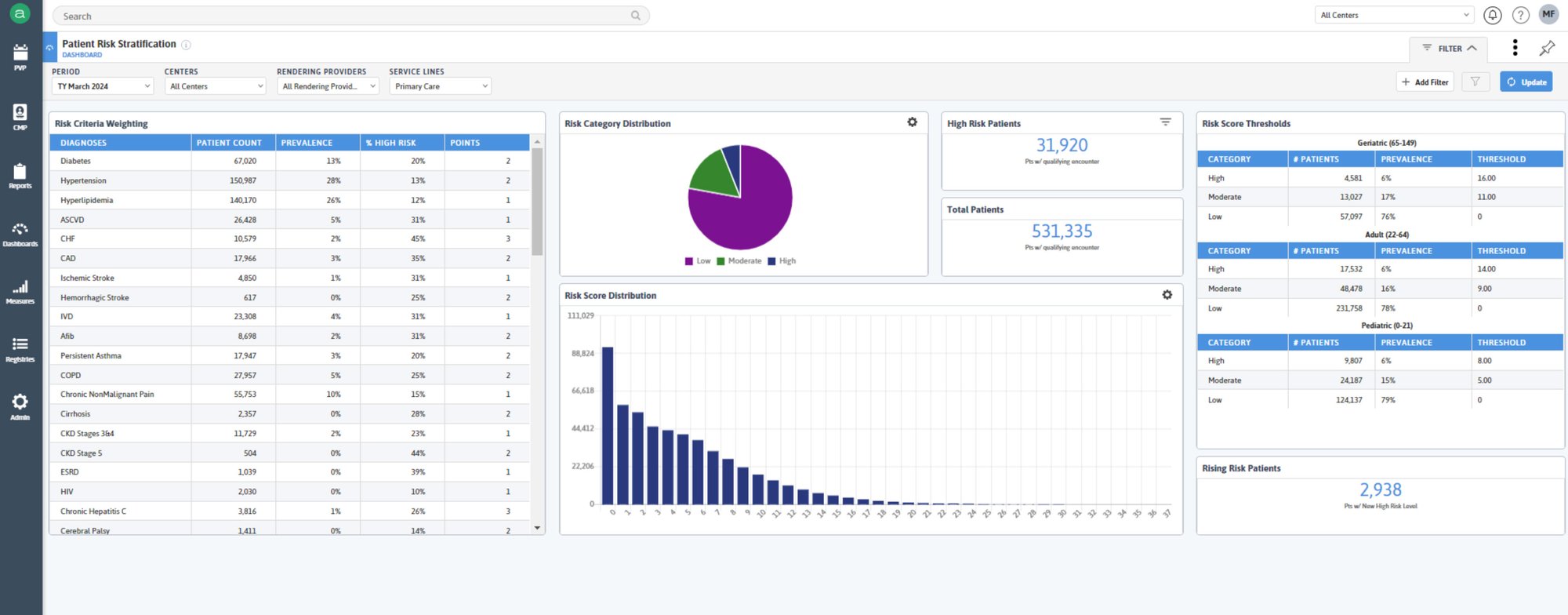
Leverage expanded clinical insights, including social determinants of health (SDOH) and demographics to optimize HEDIS measure performance and facilitate risk recapture.
Gain granular insights into cost and utilization drivers throughout the network, enabling targeted interventions to optimize performance at the network, practice, and provider levels.
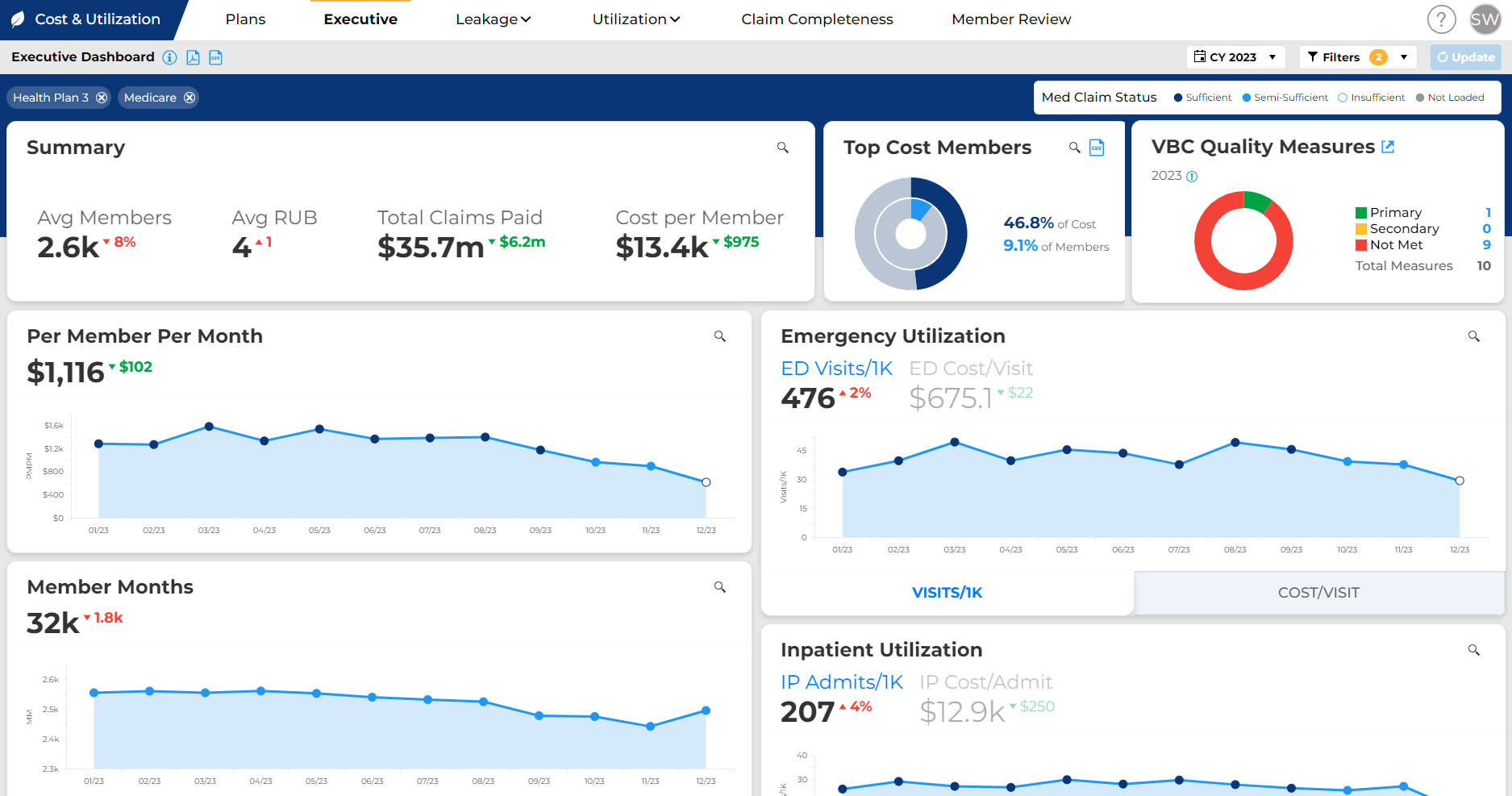
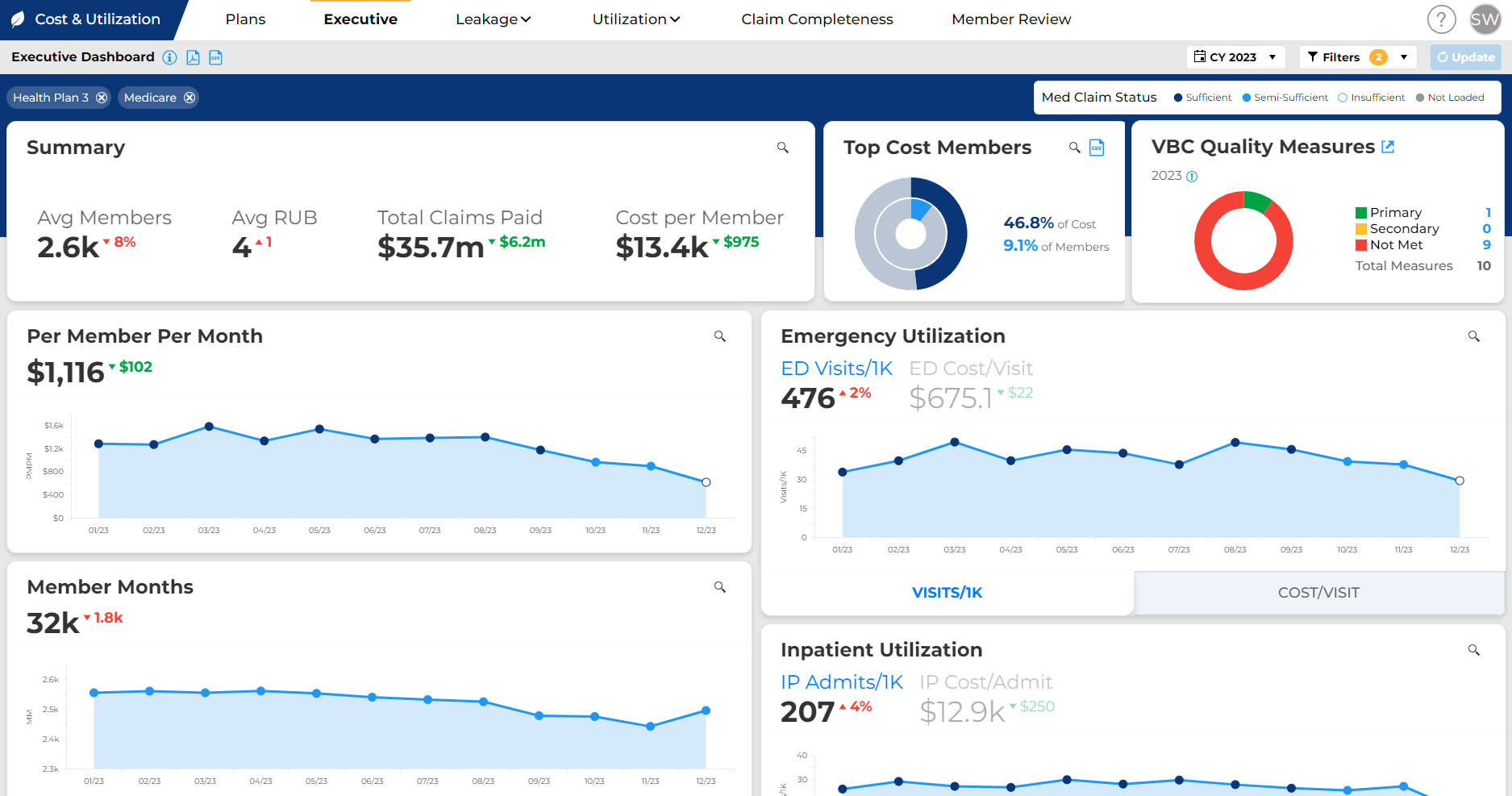

Azara DRVS empowers users to navigate the complexities of value-based care with a highly configurable and feature-rich platform, which includes:
Intuitive Dashboards
Innovative Dynamic Cohorts
Data Activation
Value-Based Care Success
NCQA Data Aggregator Validation
Azara Healthcare was part of the first cohort organizations which earned Certified Data Stream status in 2021 for NCQA’s Data Aggregator Validation Program - the highest level of certification offered by the National Committee for Quality Assurance (NCQA).
Validated data flows promote trust in aggregated clinical data. They support adoption of value-based contracting by making many of its core features more workable. This also eases the quality measurement load - validated data streams are uniquely accepted as standard supplemental data in HEDIS® audits. This means no primary source verification is required for HEDIS reporting when health plans report data from validated sources.
Validated data flows are an important, early step on the pathway to a digital measurement ecosystem.
Additional Resources
MARKET REPORT
LEARNING SERIES
SUCCESS STORY



