Wilmington Community Clinic
Wilmington Community Clinic Uses Azara DRVS to Support a New Staff Incentive Program to Help Improve Patient Outcomes and Motivate the Workforce
As the healthcare industry shifts towards value-based care, motivating health center staff to embrace more industry change can be daunting. The 1,400 federally qualified health centers across the U.S. are an essential source of primary-care services for approximately 24.3 million individuals. New payment and care models are demanding health center staff, once again, have the resiliency to improve and measure patient care, achieve new productivity and financial goals, and work more effectively as teams.
With Alternative Payment Models (APM) forcing needed changes at their clinic, the Wilmington Community Clinic (WCC) located in the greater Los Angeles area, set forth to create a staff incentive pilot program aimed at improving the lives of their patients and their workforce. Dolores Bonilla, CEO at Wilmington Community Clinic, sought assistance from health center financial experts Greg Facktor & Associates, to implement an incentive program that required dedicated time, money, communications, and data. As part of the effort, WCC utilized Azara DRVS to help with data analytics, visit planning, and dashboard creation to track the program’s quality improvement (QI) objectives.
Building an Incentive Program
According to the Incentive Research Foundation, incentive programs improve individual performance on average by 22% and within teams by 44%. Employees and managers consider incentive programs to be of high-value to an organization, yet over 98% complain about their implementation. Better yet, organizations that offer incentives attract and retain top talent – a continuous challenge in the community health sector. Given these factors, WCC wanted to create and implement a program that would keep their workforce engaged.
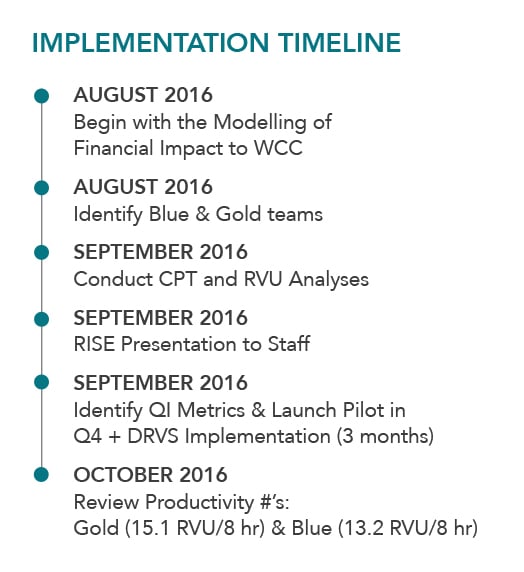
The program branded RISE or Revenue is Shared with Everyone, launched in January 2017. It required five months of preparation led by Greg Facktor & Associates, that included the careful analysis of financial impact and payout calculations based on team and individual productivity and QI performance based on a tiered scale.
Program Building Blocks
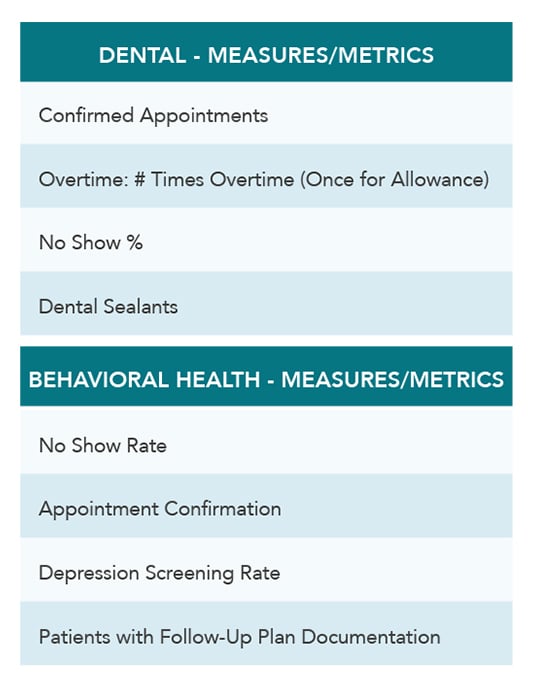
Four provider teams were identified and made up of WCC primary care, dental, and behavioral health providers and supporting and administrative staff members.
- Team GOLD
½ primary care and ½ behavioral health - Team BLUE
½ primary care and ½ behavioral health
- Team DENTAL
Dental providers and staff only - Team SUPPORT
WCC Administration, O&E, and Finance
The productivity measure equaled the average number of visits by providers for an eight-hour shift. RISE used the national benchmark of three patients per hour and adjusted for patient complexity by using Relative Value Units (RVUs) of care delivered, which allowed them to incorporate patient complexity into the productivity calculations – a much needed factor in community health.
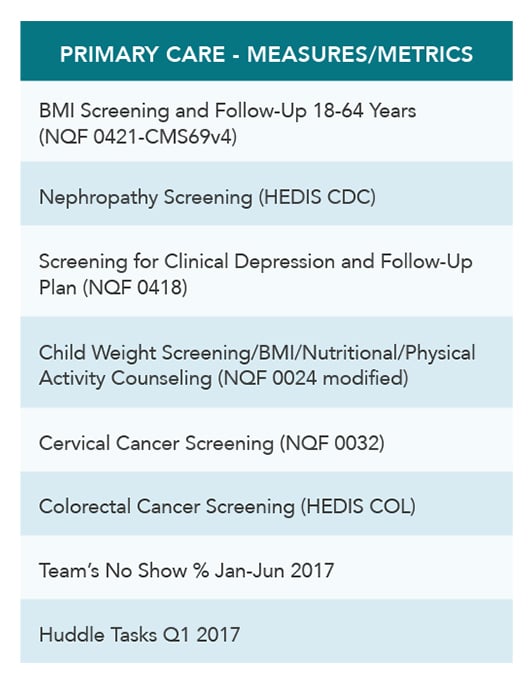
Next, WCC chose quality measures for patient outcomes determined by HRSA and CMS and allowed the team to choose relevant measures. The measures were then submitted to leadership for approval and evaluated based on two criteria. One – if they could show improvements in care quality and two – if the metric could be easily measured and trusted. Once approved, team participation and tracking went into effect.
Combining the quality measures, productivity goals, and a points-driven patient visit flash survey, program participants could earn between $200 and $1,600 per month for meeting or exceeding targets. Payouts were determined by seniority at the clinic and their full-time equivalent (FTE) status. The following are the measures and metrics set forth for the pilot.
Data Is King
The incentive program’s reporting needed to extract data from several different sources and was used to create an extensive array of dashboards driven by Azara DRVS and Tableau. The data included:
- Encounters by provider and day
- Charge data by procedure codes to load RVU’s
- Appointment data from the practice management application
- Tasks from Greenway Intergy - WCC’s Electronic Health Record (EHR) system
- Employee hours from the payroll system
- QI metrics and Visit Planning Reports from Azara DRVS
RISE Dashboard Examples
.png?width=524&name=Wilmington-Screenshot-col-1%20(1).png)
.png?width=524&name=Wilmington-Screenshot-col-2a%20(1).png)
Results
The WCC RISE program proved to be a success within six months! WCC saw an improvement in staff productivity month over month, improvements in quality measures such as BMI screening and follow up, depression screening and follow up, child weight screening and counseling, and nephropathy screening. The clinic provided over $18,000 in incentive payments to staff members for the quarter’s payouts. Team Blue, made up of ½ primary care and ½ behavioral health providers, was the pilot program winner.
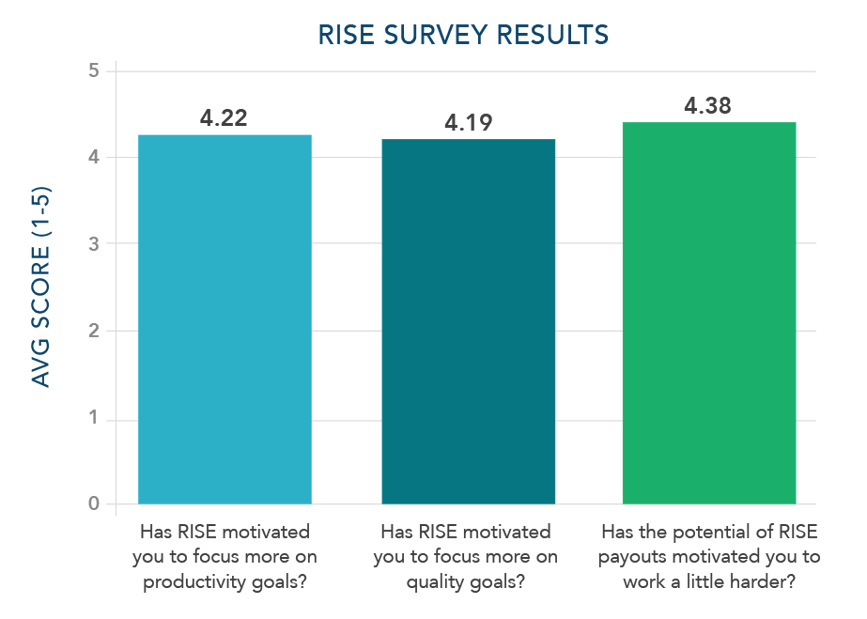
During the six-month pilot program, WCC and Greg Facktor & Associates did make slight adjustments. Team make up, program goals, and the flash survey questions were strengthened. To best manage the big changes happening at the health center, constant reinforcement of the program’s ultimate goal was continuously communicated. Dolores Bonilla also evaluated if the program motivated the staff. Using an employee feedback survey with a scale of 1-5 (1 – not at all to 5, very much), Dolores achieved what she was hoping for.
The Incentive Program Today
The initial pilot program ended in April 2017. Since then, WCC created new teams based on service lines – Primary Care, Behavioral Health, and Dental – and enhanced the hours worked requirements to account for staff covering for others. The flash survey now includes CAHPS questions used as an additional QI metric; other new QI metrics include punctuality, closure of open encounters, Title X outreach, and task completion. A Tableau dashboard is now available to showcase team and individual performance on demand and keep teams motivated with a little healthy competition. Lastly, WCC’s leaders also integrate RISE into recruitment discussions, look for more opportunities to use data to energize and optimize their center, and keep the entire workforce focused on the big picture of improving value-based patient care.
