Tiburcio Vasquez Health Center
 OVERVIEW: Tiburcio Vasquez Health Center (TVHC), a multi-site FQHC located in the San Francisco Bay-area, uses the DRVS Patient Visit Planning Report (PVP) to improve patient outcomes, clinical quality measures (CQMs) and staff satisfaction and collaboration. Part of the Azara DRVS data analytics and reporting platform, the PVP helps to ensure that no care opportunities are missed and enables all care team mem-bers to perform tasks that match their training and skill level. TVHC launched the PVP with a 12-week pilot. It included a thorough effort by center leadership and quality staff to define the roles and responsibilities of care team members. Azara provided hands-on training. The PVP boosts TVHC care team member confidence and fosters trust between providers and team members. It would not have succeeded without the support of center leader-ship, the dedication of the quality improvement (QI) staff, and the commitment of all care team members.
OVERVIEW: Tiburcio Vasquez Health Center (TVHC), a multi-site FQHC located in the San Francisco Bay-area, uses the DRVS Patient Visit Planning Report (PVP) to improve patient outcomes, clinical quality measures (CQMs) and staff satisfaction and collaboration. Part of the Azara DRVS data analytics and reporting platform, the PVP helps to ensure that no care opportunities are missed and enables all care team mem-bers to perform tasks that match their training and skill level. TVHC launched the PVP with a 12-week pilot. It included a thorough effort by center leadership and quality staff to define the roles and responsibilities of care team members. Azara provided hands-on training. The PVP boosts TVHC care team member confidence and fosters trust between providers and team members. It would not have succeeded without the support of center leader-ship, the dedication of the quality improvement (QI) staff, and the commitment of all care team members.
What is the PVP?
The PVP or “huddle report” provides actionable data listed by provider, patient, and in the order of each day’s scheduled appointments. Care team members, such as medical assistants (MAs) and licensed practical nurses (LPNs), review the PVP before and during the morning team huddle. PVP information includes:
- Patients due for preventative screenings
- Condition-relevant patient alerts, such as diabetes
A1c tests and blood pressure - Risk factors, such as smoking, obesity, and mental health
Health centers value the PVP because it aligns testing and treatment with a patient’s visit. The approach significantly decreases the likelihood of missed care steps. Patients receive important treatments and preventative screenings while they are at the health center.
Anitha Mullangi, M.D., CMO at TVHC, said the PVP provides care staff with a complete, streamlined overview of each patient’s needs. Clinicians no longer need to print several reports from an EHR to workup a patient’s comprehensive medical history or to determine whether screenings or fol-low-up care services are needed. “It’s much easier to see. It’s been a great improvement,” she said.
The PVP also helps providers streamline care team communication. They can untether themselves from tasks that are more appropriate for other team members. Providers benefit from more exam room time with patients, where they can educate and motivate them about changes that can improve their health.
Key PVP Objectives and Outcomes
- Optimize Treatment for Patients
Data available to care team at time of visit - Emphasize Time for Relationship
Provider better engages patient in care - Increase Staff Satisfaction
Smoother days for providers and support staff - Better Access and Efficiency
Unnecessary appointments and phone calls eliminated - Improve Measure Performance
Quality improvement care gap review baked in at point of care; missed opportunities avoided
Pilot Lays Groundwork For Success
Andrea Schwab-Galindo, TVHC’s chief administrative officer, said the center sought a tool that could improve patient health outcomes, lower costs, enhance the patient experience as well as the care team’s experience. It also had to be easy to use and accessible to the whole center.
“We wanted a tool that anyone, from an administrator, to a clinician, to a busy provider, could jump right into and run a report,” she said.
For the pilot’s first seven weeks, TVHC leaders tailored the PVP to meet the center’s needs. They chose which clinical quality measures (CQMs) to include and determined care team member roles and responsibilities. Leaders also made important decisions about standing orders and standing actions. Then, Azara led a daylong, staff-wide training session. Care teams participated in exercises and discussions that addressed value-based care and visit planning improvement. Medical assistants (MA), LPNs and other care sup-port team staff received hands-on PVP training and joined providers for mock care team huddles.
Some of the training exercises identified incorrect assumptions team members had about others’ roles and responsibilities. In one exercise, participants placed jellybeans in cups marked with care team roles, such as MA and RN. The jellybeans represented the effort associated with care tasks by care team members. Participants’ decisions on where to place the jellybeans revealed how well the team was or was not spreading the tasks across team members before stand-ing orders and changes in roles/responsibilities associated with the pilot were implemented. The activity helped build the will for change.
Key Quality Measures Rise as Center Embraces PVP
Multiple factors contributed to the pilot’s success. TVHC leadership strongly supported the initiative; additionally, the quality improvement (QI) team worked with staff on a one-to-one basis, which ensured that the care teams used the PVP consistently and properly. The center’s sites significantly improved clinical quality measures (CQMs), including screening for cervical cancer, colorectal cancer, and depression. Care staff at each site streamlined their workflows and collaborated more effectively.
Additional Takeaways:
- Improved staff collaboration allowed the providers to spend more time with their patients. They were more comfortable delegating work to their nurses and medical assistants.
- Care team staff members are determined to succeed with the PVP. They are excited to be part of a team effort and get excited about the care improvements.
- PVP expansion is planned. The tool was first implemented at TVHC’s Union City site, and later in nearby Hayward. Rollout continued in San Leandro and at the new Firehouse Clinic in Hayward. It will also be expanded to other parts of the organization, including behavioral health providers and administrative staff.
Conclusion
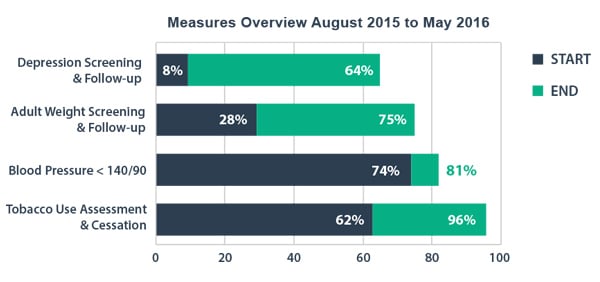
TVHC’s PVP pilot, bolstered by the commitment of center leadership and QI oversight, has improved patient outcomes, staff collaboration and center efficiency. The pilot and expansion also helped improve staff retention of providers as well as support team members. In environments where CHCs are battling with private practices for staff, retaining staff through satisfaction and efficiency is critical. Additionally, several key quality measures rose significantly by the end of the 12-week project, but even more impressively, the graphic shown represents the pilot and expansion teams’ performance over 10 months, during which the teams maintained the gains from the pilot, and went on to surpass them. These results are a real tribute to the dedication of the care team members at Tiburcio Vasquez Health Center, their leadership, who supported and fostered the project, as well as the report and new processes being used to facilitate efficient accurate care for patients when they come in for a visit.
Kaiser Permanente, CPCA Fund Pilot: The Community Health Care Network (CHCN), a health center consortium that operates under the California Primary Care Association (CPCA), used funding from Kaiser Permanente’s PHASE (Prevent Heart Attacks And Strokes Everyday) program to pay for the pilot at the Union City center site; CPCA funded training the sites in Hayward and San Leandro.
