DotHouse Health
Scaling New Heights: DotHouse Health Boosts Quality, Fosters Teamwork With Help From Azara DRVS And ‘Mountain Climbers’
IN BRIEF: DotHouse Health, a federally qualified health center in Boston’s Dorchester neighborhood that serves more than 20,000 low-income patients, implemented Azara DRVS in 2014 as part of its effort to satisfy its ever-increasing demand for accessible, actionable data. The health center’s quality improvement team used some arts and crafts skills to boost the transparency of several clinical quality measures. As a result, DotHouse is having some fun with its data while fostering meaningful collaboration among its care team members. Key quality measures are rising, and some have already surpassed the health center’s annual goals.
20,000 low-income patients, implemented Azara DRVS in 2014 as part of its effort to satisfy its ever-increasing demand for accessible, actionable data. The health center’s quality improvement team used some arts and crafts skills to boost the transparency of several clinical quality measures. As a result, DotHouse is having some fun with its data while fostering meaningful collaboration among its care team members. Key quality measures are rising, and some have already surpassed the health center’s annual goals.
THE STORY: Once a month Laura Santel and Quyen Pham trek to construction paper-clad bulletin boards that are perched in the hallways DotHouse Health, a community health center in Boston’s Dorchester neighborhood: it’s time for them to move the mountain men.
Santel, the center’s clinical project manager, and Pham, its quality and reporting coordinator, bump smiling climbers further up the sides of paper mountain peaks. Each mountain represents one of the center’s key clinical quality measures, such as its screening rate for colorectal cancer.The nearer a climber gets to a summit, the closer DotHouse is to reaching an annual quality target.
The cheerful display is a fun, eye-catching and highly visible approach to keeping the care staff apprised of performance and for encouraging teamwork and some friendly competition.
“Over the years, we’ve given providers data in many different formats,” said Santel. “We used to send monthly emails with links to 30 different reports, but those were difficult to absorb. We wanted to provide the care teams with something that engaged them and encouraged them to work together. We needed more than a chart, so we came up with the mountain climbers.”
DotHouse, which provides care to more than 20,000 residents, most of whom receive Medicaid, grapples with a heavy thirst for data. The federally qualified health center (FQHC) must adhere to stringent data reporting requirements, such as annual Uniform Data Set (UDS) measures required by the Health Resources and Services Administration (HRSA). As a patient centered medical home (PCMH), DotHouse also produces numerous data reports for its accountable care organization (ACO) payment contracts.
External reporting needs aside, DotHouse must fulfill its hefty internal data needs. Its in-house reporting team struggled to meet the demand for reports and data-related questions from staff. It needed a fast, robust platform that could transform vast amounts of patient information into meaningful, actionable data. In January 2014, it implemented Azara DRVS to help satisfy those needs.
Results are positive thus far, as DotHouse’s quality and clinical staff have developed effective new methods for extracting and analyzing data. They can wrangle the data they need in a timely fashion.
“DRVS allows us to work more independently and to perform the ad hoc analysis we need,” said Santel.“The data is readily accessible to everyone who wants it. It’s very user-friendly.”
In addition to the mountain men boards, which display the center’s overall performance on key measures, another set of boards compares the performance of different care teams. DotHouse’s adult medicine practice has four teams; the family medicine practice has two; pediatrics has three. Each team consists of two to four providers; each provider is paired with a medical assistant; a nurse supports each team; a care coordinator serves two teams.
“We’re trying to get staff more engaged with the data and to show them their performance numbers so that they are more incentivized to improve,” said Pham. “We have also seen some friendly competition among providers, which helps to improve their numbers.”
Special scorecards managed through DRVS are used to track individual provider performance on key quality measures, but that information is not shared publicly with the rest of the center.
DotHouse Brings Quality Measures in Focus with DRVS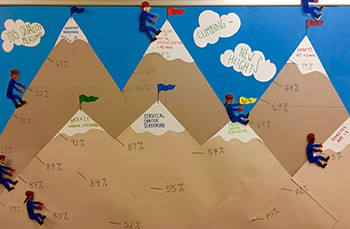
With DRVS up and running, DotHouse focused on improving seven quality measures in 2015. They include: screenings for colon, cervical and breast cancers; hemoglobin A1c < 8; diabetes A1c tested every six months; and follow-ups with patients in less than 48 hours post-emergency room visits and hospitalizations.
Some providers were surprised to learn they lagged behind their peers on key measures. But the problem – in many cases – was not that they provided inadequate care. Rather, they did not properly document the care provided in the center’s electronic health record (EHR). For example, colonoscopy reports were often scanned into the EHR, a method that fails to get recorded as structured data.
All of the care teams chose to pay close attention to the center’s colorectal cancer screening rate because it was DotHouse’s worst performing measure. The quality and clinical staff developed new workflows designed to boost the screening rate. Among them, medical assistants now offer patients who are unwilling or unable to get a colonoscopy an at-home FIT test kit so that they can still be screened for colorectal cancer.
Efforts have paid off. DotHouse began 2015 with a 49 percent colorectal cancer screening rate, and aimed to hit 60 percent by year’s end. The center eclipsed its annual goal by May, hitting 64 percent.
Other measures have also exceeded annual goals, including hemoglobin A1c tested every six months.
Boosting Measures Through Visit Planning and Care Coordination
In addition to tracking quality measures with DRVS, DotHouse has begun to roll out the platform’s Patient Visit Planning Report (PVP), which provides the clinical staff with a streamlined, comprehensive tool for managing each day’s slate of patients. The medical assistants, who are the PVP’s main users at the FQHC, can view all the tests a patient is due to receive during a particular visit, learn of any risk factors, determine whether lab tests should be ordered, and review other information designed to ensure each patient receives complete, appropriate care.
Santel and Pham said that center’s physicians find the PVP helpful because it decreases their workload and allows them to spend more time treating their patients.
“If we didn’t have something like this, we’d have a lot of missed opportunities,” said Santel.
The PVP exemplifies Dot House’s effort to expand its team-based care. The providers and medical assistants provide the hands-on care, and a team of care coordinators review the center’s entire patient panel to ensure patients receive care at regular intervals. The combined effort helps to improve the center’s overall performance and to enhance meaningful collaboration among the staff. Pham said providers often complement medical assistants and other staff for their efforts to improve patient care. The mountain climber boards have helped to bring those efforts into focus and to provide staff with a common rallying point.
“It’s hard to see wins sometimes, so I think this is a small way that you can see that the team worked together and made numbers go up,” she said. “Moving those little guys up the mountains takes a lot of work.”
