A few weeks ago, LuAnn Kimker wrote about “The New Normal” for providing care in the health center setting and the quick pivot to integrate telehealth into daily care routines during the time of COVID-19. Suddenly, health centers’ usual Plan-Do-Study-Act cycles have been dramatically accelerated, and there’s so much to adapt to on a daily basis as the situation evolves and the guidelines for care delivery and reimbursement continue to change. In our conversations with so many of you, we have been impressed with all the adaptations you have already made. The ability to quickly respond to the changing environment is one of the distinguishing traits of health centers throughout their history, and you have proven that continues to be true.
We are aware of concerns about not seeing patients face-to-face and how to shift the role of support staff and others, such as dental providers, to work that fulfills the needs of patients but also helps the health center continue to stay financially sound. It sounds so harsh as I write it, but I know for many of you it’s the reality, and so many have been faced with very painful decisions in these past weeks. Many of you are already trying new approaches and have been generous enough to share those ideas with us. In addition to your suggestions, we’ve come up with many opportunities for re-purposing existing roles and adjusting tasks. For those of you who had the opportunity to attend our webinar last week, you know the first half focused on our ideas in this area. If you missed it, you may want to check it out here.
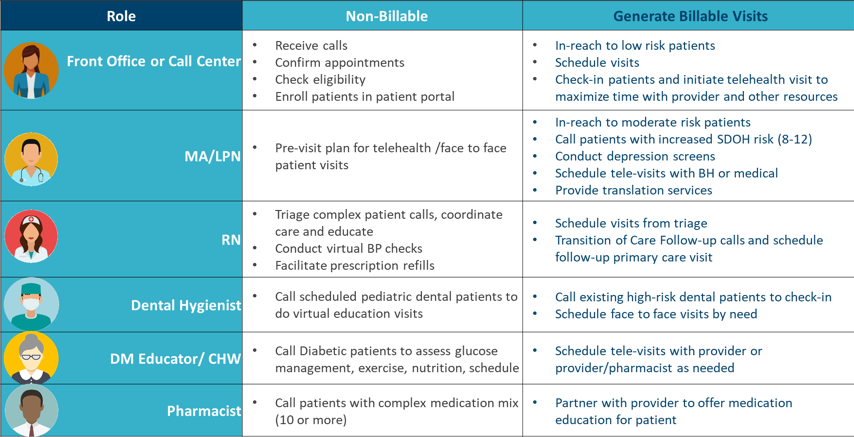
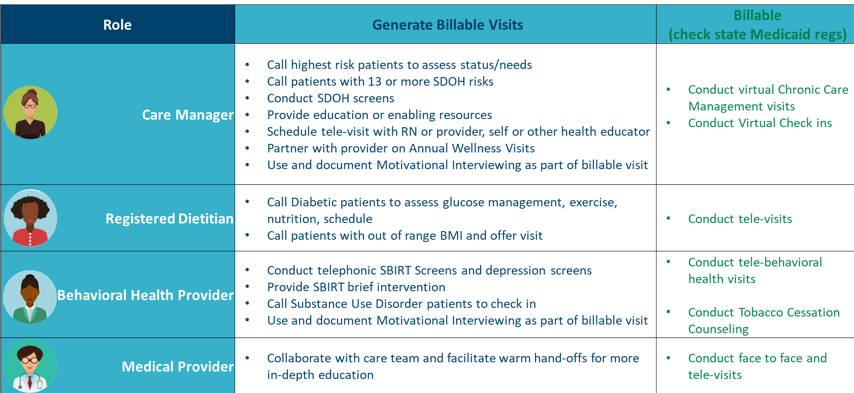
In this presentation, we gave an overview of typical roles and tasks on health center teams, and how those staff can continue to contribute in a myriad of ways — some non-billable, some generating billable visits, and some billable with the relaxed telehealth reimbursement rules. So many patients have both new and on-going needs that provide an opportunity for you to utilize staff in unconventional ways to provide high quality care to your patients.
There are some key benefits of connecting with patients in a much more proactive, outreach-driven way. First, it allows you to let patients know what kind of care they can receive from you at this time. Many of them would not imagine your new capacities to see them curbside, via telephone or video, or to be supported in a myriad of other ways.
This is also an opportunity to engage with your patients in a new way and really build your relationships with them. Patients appreciate being checked on under these circumstances, especially if they are vulnerable in any way. Outreach also gives you a chance to listen in a new way. What are your patients saying they need now? How might what you hear change the programming you design or the services you provide now?
This is also an incredible opportunity to collect valuable data that we often struggle to find time to provide in the traditional setting: Social Determinants of Health (SDOH) screens, Screening and Brief Intervention (SBIRT) screens, substance use and dependency screens, patient portal enrollment, and depression or anxiety screenings. Given all the financial uncertainty, job furloughs and losses, this is a time of acute distress for many people, and screening people for depression and anxiety is a way to find out who needs a visit with your behavioral health providers, especially since so many of you adeptly shifted your behavioral health services to phone and video.
The first table below contains suggestions for ways to utilize traditionally non-billable staff in patient engagement, outreach, and the generation of potentially billable visits. Many of these staff may be essential for making billable visits possible. For example, a provider may need the translation services of a medical assistant to see patients who speak a language the provider does not.
Table One
The second table consists of traditionally billable providers and allowable billable activities according to Medicare. Please check your individual state regulations to understand what kinds of visits are billable in your state as telehealth, if there are requirements regarding phone or video provision, as well as what codes may be used for charges. We recognize these are both incomplete lists, but they are a good place to start if you or your practice need help thinking about how your staff can help you meet patients where they are.
Table Two
Traditionally, health centers have not been keenly focused on proper billing practices because of the benefit of encounter rate billing, which does not incent detailed charges. For this reason, many health center providers are not given adequate billing training. This crisis demands specific attention be paid to the appropriate Evaluation and Management (E&M), Current Procedural Terminology (CPT) codes and modifiers that may be used for telehealth in your environment. Getting properly reimbursed for the work you do is more essential than ever.
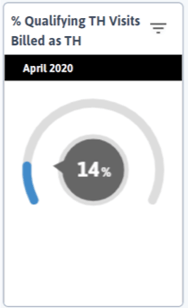 Azara has recently added new functionality to help you track telehealth visits — including those patient interactions you consider “telehealth” and what percentage of those have telehealth charges associated with them. You may be interested in seeing a widget that expresses this idea on the Telehealth Expansion and Mapping Dashboard, under the Custom Dashboard Menu. Look for the widget pictured on the left: “% Qualifying Telehealth Visits Billed as Telehealth.” The goal of this widget is to expose the opportunity that exists to submit charges for qualifying telehealth visits. To review how to map telehealth interactions in the DRVS mapping administration tool please refer to this Quick Tip Clip.
Azara has recently added new functionality to help you track telehealth visits — including those patient interactions you consider “telehealth” and what percentage of those have telehealth charges associated with them. You may be interested in seeing a widget that expresses this idea on the Telehealth Expansion and Mapping Dashboard, under the Custom Dashboard Menu. Look for the widget pictured on the left: “% Qualifying Telehealth Visits Billed as Telehealth.” The goal of this widget is to expose the opportunity that exists to submit charges for qualifying telehealth visits. To review how to map telehealth interactions in the DRVS mapping administration tool please refer to this Quick Tip Clip.
Once we emerge from our current state of response to COVID-19, we expect many aspects of the new normal will be with us for a long time. Patients will likely expect us to continue delivery care via telephone and video, because for so many patients it’s so much more convenient. Depending on the region, we are aware that some states struggle with reliable internet service, and of course it’s still a reality that many of our most vulnerable patients don’t have access to computers or smart phones. There is more work to be done to solve some of these problems, but the progress we have made and the creativity, energy and courage you all have demonstrated is so inspiring! When you are ready to consider how we incorporate telehealth for the long term please check out this article The Transition from Reimagining to Recreating Health Care is Now from NEJM Catalyst.
Finally, please join us again this Thursday 4/16 at 1pm ET to for a new webinar: Deep Dive on New Care Delivery Paradigms, to learn more about what is possible in telehealth and staff re-deployment from your peers, along with some exploration of additional tracking tools from Azara.
