You read it in the news headlines. You see it across social media. You hear in healthcare conferences and press conferences alike. It seems like everyone is talking about it. No, it’s not the latest meme or viral trend; it’s the concerning uptick in syphilis infections across the country. Syphilis is a sexually transmitted infection (STI) that is spread through direct contact of a syphilis sore during sex or from a mother to her unborn child.
In its primary stage, syphilis presents as sores or rashes where syphilis entered the body (in places like the genitals or mouth). While the sores are typically painless and will go away after a few weeks, the syphilis bacteria remains in the body and can infect others or reappear. If not treated, the secondary stage of syphilis reveals itself with the reappearance of sores or rashes, with additional symptoms common with infection, like fever, swollen lymph nodes, and sore throat. At this stage treatment is needed for the infection to go away. While uncommon, the tertiary stage of syphilis affects different organ systems across the body like cardiovascular and nervous systems and can result in death. Despite the relative ease of transmission, syphilis can also be easily treated with antibiotics.
Syphilis is top of mind for healthcare professionals across the country as both syphilis and congenital syphilis rates have seen a significant increase in the last decade. There was a 31.9% increase in syphilis from 2020 to 2021, despite the COVID-19 pandemic shuttering many testing sites. In the last 5 years, syphilis rates increased 78.9% and congenital syphilis increased 183.4%. These trends are especially concerning in the American Indian and Alaskan Native (AI/AN) communities, who saw a 520% increase in rates of primary and secondary syphilis between 2016 and 2021. Congenital syphilis rates have also been increasing every year since 2013. AI/AN communities have seen a 900% increase in the rates of congenital syphilis in their communities which is almost 10 times higher than the white population.
One of the most critical steps in preventing the spread of syphilis is early testing and treatment of individuals who are infected. The United State Preventive Services Task Force (USPSTF) recommends screening for syphilis infection in persons who are at increased risk for infection. This includes factors such as community prevalence and behavioral risk factors such as men who have sex with men (MSM), individuals who are HIV+, individuals engaged with the justice system or those who engage in sex work. USPSTF also recommends early screening for syphilis infection in all pregnant individuals. If the person who is pregnant also has other risk factors (like community prevalence, incarceration status, HIV status), USPSTF also recommends a re-screen for syphilis in the early 3rd trimester and again at delivery.
With the increased importance of screening and treatment, how can we use data to identify patients who need a syphilis test? Azara DRVS!
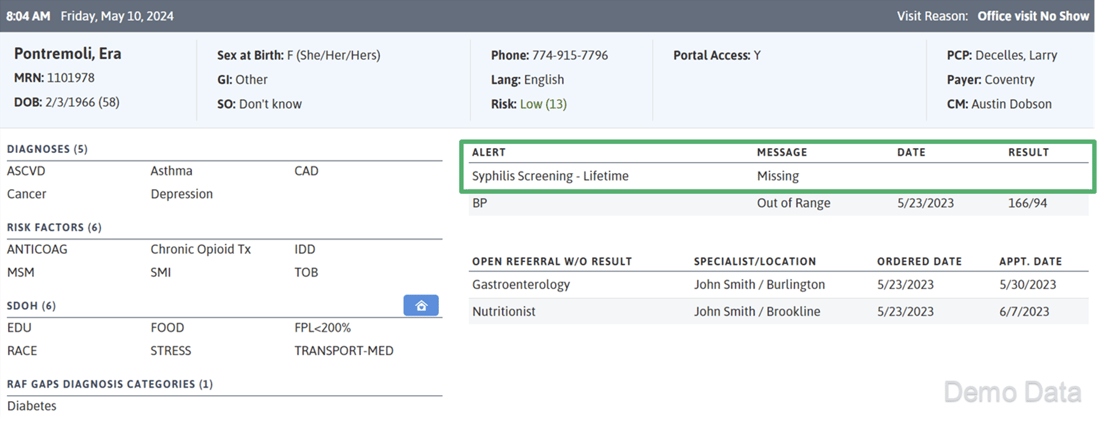
Using the Patient Visit Planning report (PVP), care teams are easily able to see who needs a screening. In the core DRVS platform, there are three alerts for identifying patients in need of a syphilis screen at the point of care:
- Syphilis Screening Lifetime: Alert will trigger if syphilis screening has not occurred in the last 100 years. Alert only applies to female patients >= 18 years old.
- Syphilis Screening - 1st Trimester: Alert will trigger for patients who are pregnant and missing a syphilis screening during their first trimester. This alert is not configurable.
- Syphilis Screening - 28 Weeks Gestation: Alert will trigger for patients who are pregnant and are missing a syphilis screening at or after 28 weeks gestation. This alert is not configurable.
Additionally, practices can track ordered and completed syphilis labs in the Open Lab Orders and Completed Lab Volume measures. To pair syphilis testing and results with other risk factors like pregnancy, HIV status, and incarceration history, consider creating a custom registry and adding all the data elements or columns you would want to consider when prioritizing patients for screening.


For practices with the DRVS HIV Add On Module, there are additional tools to track syphilis screenings for patients with HIV. On the Patient Visit Planning report, care teams can identify patients with HIV who have not had a syphilis screening:
- Syphilis Screening - Initial HIV Dx: Alert will trigger for patients with an initial diagnosis of HIV in the past year who have not had a syphilis screening on or after diagnosis date. This alert is not configurable.
- Syphilis Screening - HIV: Alert will trigger if syphilis screening has not occurred in the last 6 months. Patient must have a diagnosis of HIV.
There are also 2 measures to track the percent of patients with HIV who have received a syphilis test and to track treatment of patients with HIV who had a positive syphilis test.


To address the rising rates of syphilis across the country, practices must leverage data to identify patients at risk and in need of a screening. By using tools in Azara DRVS like the Patient Visit Planning report to alert care teams, and measures and registries to track results and treatment, organizations can make an impact in the syphilis prevalence in their communities.
Related Articles

Keeping Care Close to Home: How Azara Empowers Rural Providers
Explore Insights
From Silos to Solutions: Advancing Behavioral Health Integration in Primary Care
Explore Insights
