Influenza, or the flu, is a virus that impacts tens of millions of Americans each year. For most, the flu is an inconvenience—something that knocks you down for a few days and makes you feel crummy. But for some, including children, elderly, and the immunocompromised, the flu can be very serious, causing hospitalization and even death. Peak flu season varies year to year but occurs most often between December and February, with the flu “season” running from October to April. During the 2023-2024 flu season, the CDC estimates that 40 million people were sick with influenza, 18 million people visited a healthcare provider for influenza, 470,000 had influenza-related hospitalizations, and 28,000 influenza-related deaths occurred.
Despite the heavy burden of influenza each year, there are ways to reduce its impact on individuals, the community, and the healthcare system. One critical way to mitigate the risk of influenza is the flu vaccine. Each year, scientists develop new flu vaccines to tackle the evolving virus, with as many as 148 million doses of influenza vaccines prepared for the 2023-2024 season. And for those who receive a flu shot, the vaccination can help prevent infection and reduce the severity of symptoms, especially in at-risk populations. During the 2023-2024 flu season, the CDC estimates that the flu vaccine prevented 9.8 million influenza-related illnesses, 4.8 million medical visits, 120,000 influenza-related hospitalizations, and 7,900 influenza-related deaths. Research has found that flu vaccines reduce the risk of an influenza infection by 40-60%.
Fun Fact: FQHCs connected to Azara DRVS have administered nearly 1 million influenza vaccines so far this flu season!
Despite the benefits of the flu vaccine, only about half of Americans get their annual flu shot. What’s even more concerning is this number is trending downward. During the 2023-2024 flu season, the CDC estimates that flu vaccination coverage among all people six months and older was 47.2%, and this is 2.1 percentage points lower than the previous season. While not a significant decrease, this trend reflects larger, more troubling trends around growing vaccine hesitancy across the country. Rates of childhood immunizations are still struggling to rebound to their pre-COVID rates – 2023 UDS immunization rates were down 3% compared to 2022. Adolescent and adult immunizations also are on the decline, with flu vaccination rates at or below pre-pandemic levels for both commercial and Medicaid patients. Other common challenges for increasing immunization rates include documentation issues and the inability to identify patients needing vaccines.
Vaccine hesitancy is a complicated issue which can be addressed, but requires sensitivity and community-specific awareness. One study on childhood immunization rates and vaccine hesitancy found that vaccine-hesitant parents far outnumber vaccine refusers. This group may be more open to discussions about the importance of vaccines, and primary care providers play a key role as a trusted source of medical information.
As a leading population health management tool, DRVS provides functionality to identify, engage, and track patients needing influenza vaccines and those with an influenza-like illness (ILI). With a proactive, streamlined approach to meeting the needs of patients and communities, care team members can spend more time developing relationships with patients and their families, becoming a trusted source of medical information.
Identify
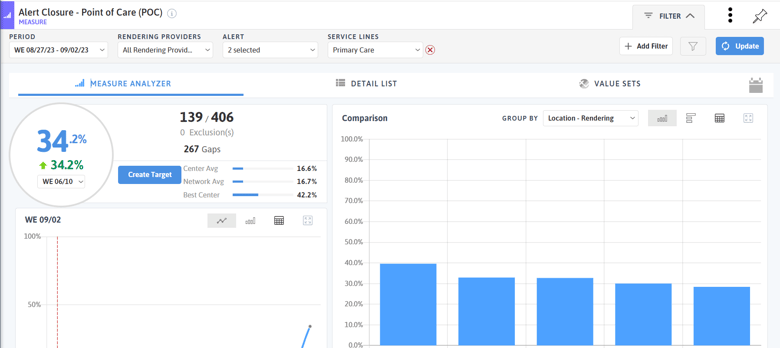
At the point of care, Azara DRVS users can leverage the Patient Visit Planning (PVP) report to identify individuals who are due for their flu shot. There are three alerts available to enable on the PVP: CDC Immunization Flu (for children 6 months to 8 years old), Flu - Annual, and Flu - Seasonal. The seasonal flu alert looks for vaccinations between August 1st and May 1st. We recommend only enabling the Flu - Seasonal Alert when you have doses to give. To spark competition across care teams or locations, use the Alert Closure - Point of Care measure to track the percentage of flu shots completed each day or each week.
For a population-level approach in identifying patients who are due for a flu vaccine, use the gaps on the detail list of the Influenza Immunization - Year Only measure or a registry that contains information on historical flu vaccines. The Flu - Adult, Primary Care Adult, Primary Care Pediatrics, Asthma, and Diabetes registries all contain information on flu shots, or you can create a custom registry to track populations of interest, such as patients who are actively pregnant or who are immunocompromised.
Use the Influenza-Like Illness (ILI) Surveillance measure to identify patients with signs and symptoms of influenza-like illness, including fever, cough, sore throat, or upper respiratory infection. This measure excludes patients who had an assessment for strep pharyngitis or evidence of a COVID-19 diagnosis at the visit. The ILI Surveillance measure can also be leveraged for health department reporting required of the practice.
Engage
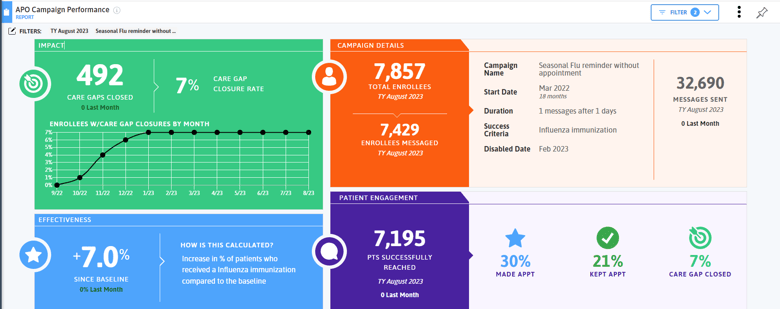
To quickly engage with individuals due for their flu shot, practices with Azara Patient Outreach can enable the Seasonal Flu campaign to text patients who are due for their annual dose. Other campaigns like Childhood Immunizations, Adolescent Immunizations, and COVID-19 Vaccinations can also be enabled to increase other vaccination rates. Practices have the ability to prioritize campaigns so patients aren’t inundated with messages.
A key part of vaccination acceptance is culturally appropriate education and care. Use filters and grouping options on the Influenza Immunization - Year Only measure to tease apart trends by different patient populations such as race, ethnicity, language, or social drivers of health. For example, if you identify that your population of patients experiencing homelessness has a lower vaccination rate than your general population, consider outreach activities like vaccination vans that target this population.
Track
To understand the impact that your practice has on your community, use the visualizations available on the influenza measures to track increases in the number of vaccinations administered and the percentage of patients who have received an annual flu shot. The Influenza Vaccines Administered measure can be run weekly or monthly to track the number of doses delivered to patients and the Influenza Immunization - Month measure can be used to track patient compliance in the short term.
Utilize Available Resources
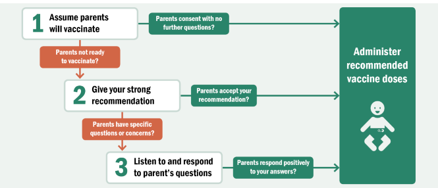 Immunizations are one of the greatest public health victories of the 20th and 21st centuries. There are many resources available for increasing vaccinations and reducing vaccine hesitancy in parents and individuals. The CDC has resources for provider conversations with parents. Also see the National Minority Quality Forum’s Center for Sustainable Health Care Quality & Equity’s “DRIVing Equity in Flu Vaccination” course on increasing flu vaccination rates and addressing disparities or check out Health Champions for resources on vaccinating patients with chronic conditions like hypertension. Access community engagement resources from the Vaccine Equity Cooperative.
Immunizations are one of the greatest public health victories of the 20th and 21st centuries. There are many resources available for increasing vaccinations and reducing vaccine hesitancy in parents and individuals. The CDC has resources for provider conversations with parents. Also see the National Minority Quality Forum’s Center for Sustainable Health Care Quality & Equity’s “DRIVing Equity in Flu Vaccination” course on increasing flu vaccination rates and addressing disparities or check out Health Champions for resources on vaccinating patients with chronic conditions like hypertension. Access community engagement resources from the Vaccine Equity Cooperative.
Practice preventive health and get your flu shot today!
If you are using DRVS tools to improve vaccination rates in your community, we would love to hear from you in our new Achieve Celebrate Engage (ACE) program here.



