Chronic disease. This is one of the biggest health challenges the United States faces as a nation. Despite some pockets of success in population health designed to manage chronic disease, as a country and as a system, we are failing. Compared to our global peers, the U.S. spends more on healthcare than almost every other nation, sometimes double or triple per person. Our life expectancy is 4-5 years lower than well-performing countries; we have some of the highest chronic disease rates in the world; and we are wasting billions of dollars treating the negative impacts of preventable and manageable chronic disease.
The good news is there are three positive trends emerging in population health for 2018 that will hopefully continue to drive needed improvement in our healthcare system.
1. Payer-Provider Collaboration
 There have been pockets of success in payer-provider collaboration for several years (like a primary care quality program in Louisiana), but none that could be considered wide-ranging or broad success. Recently, the National Committee for Quality Assurance (NCQA) added a Population Health Management (PHM) category which represents a shift from the evaluation of single-disease state toward a whole-person focus. For 2018, health plans must both describe their strategy for addressing the needs of members and demonstrate effective execution of that strategy.
There have been pockets of success in payer-provider collaboration for several years (like a primary care quality program in Louisiana), but none that could be considered wide-ranging or broad success. Recently, the National Committee for Quality Assurance (NCQA) added a Population Health Management (PHM) category which represents a shift from the evaluation of single-disease state toward a whole-person focus. For 2018, health plans must both describe their strategy for addressing the needs of members and demonstrate effective execution of that strategy.
These updated standards for wellness and complex case management now also recognize the important role of data analytics for identifying patient needs, resource targeting, and impact evaluation. This new PHM standard is designed to drive integration across providers, practices, and health plans and in support of more complete, effective, and integrated patient care.
2. Use and Evaluation of Broader Data Sets
 Many healthcare providers are using software and services to take a deeper look at their EMR and other data in order to maximize their performance across MIPS and other quality measures.
Many healthcare providers are using software and services to take a deeper look at their EMR and other data in order to maximize their performance across MIPS and other quality measures.
Often the data exists, but many EMRs (which were hastily installed during the meaningful use boom) do not produce the proper codes (i.e. quality data codes) needed for quality measures. Therefore, to achieve the correct performance and drive maximum reimbursement across both CMS (Centers for Medicare & Medicaid Services) and health plan driven quality measures, care and effort must be taken to collect and analyze patient data across multiple sources to improve care. Additional effort is often needed to extract a complete set of data in order to evaluate and leverage this information for improved patient outcomes.
3. Understanding Social Determinants of Health and Patient Behaviors
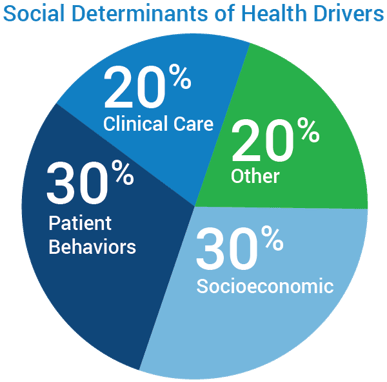 Taking care of the patient does not stop once they leave the clinic. In fact, only 20% of health outcomes are determined by clinical care. A large portion of overall health outcomes are driven by patient behaviors (30%) like medication compliance and diet, as well as socioeconomic determinants of health (30%) such as food, housing, access to transportation, education, and employment.
Taking care of the patient does not stop once they leave the clinic. In fact, only 20% of health outcomes are determined by clinical care. A large portion of overall health outcomes are driven by patient behaviors (30%) like medication compliance and diet, as well as socioeconomic determinants of health (30%) such as food, housing, access to transportation, education, and employment.
Until relatively recently, these determinants outside of clinical care were typically ignored or not managed in a way to optimize outcomes. However, there is an increasing focus on social determinants of health and patient behaviors data within the healthcare community, and there are a growing number of initiatives being developed to address these social and behavioral determinants impacting health. More healthcare organizations are adopting predictive modeling tools that help identify and aggregate social and behavioral determinants. Healthcare organizations can leverage this information to gain valuable insight into their patients’ health determinants and develop more effective care plans for the individual patient. By gaining a more comprehensive understanding of the factors impacting a patient’s health, healthcare organizations are better prepared to influence quality outcomes and provide value-based care.
Driving Healthcare Improvement for a Positive Future
Hopefully, these trends in population health for 2018 will continue to drive clinical and financial enhancements needed for improving our nation’s healthcare system and patient health outcomes. Individual healthcare organizations can play an important role in helping to improve the quality of care for their patients and members by adopting these initiatives.
For many organizations, this can be challenging. SPH Analytics works with hundreds of healthcare organizations throughout the nation, and we understand the complexities involved. We partner with healthcare providers to integrate full-service solutions to address the challenges of implementing and managing value-based programs and their complex components. Through these partnerships, we are able to observe that the most successful organizations have learned the value of payer-provider collaboration and how to effectively engage their patients, aggregate a comprehensive set of health data, and leverage this information to make a measurable impact on healthcare improvement.
By working together toward a common goal of improved healthcare for all, adopting these positive trends, and using meaningful data to drive positive outcomes, the future of healthcare in the U.S. begins to look positive.
Learn More:
Azara Healthcare and SPH Analytics Population Health Division Announce Merger
Related Articles

Navigating the Social Care Landscape: Five Lightbulb Moments from the SIREN National Research Meeting
Explore Insights
From Silos to Solutions: Advancing Behavioral Health Integration in Primary Care
Explore Insights
